What experts are saying about the flu-COVID-19 “twindemic”
In 2020, the news broke that the Pfizer and Moderna SARS-CoV-2 vaccines had reached historic milestones. This began the conversation about a roll-out plan and how our lives would be impacted moving forward. At that point in time, many schools around the US were still closed, many workers were still remote and mask-wearing restrictions were firmly in place throughout many businesses.

Since then, vaccines have become available to everyone five years of age and older, and experts estimate that sixty-two percent of people in the United States have been fully vaccinated. Unfortunately attempts to fully re-open have been curtailed around the world due to the emergence of highly transmissible variants.
Although COVID-19 cases surged during the traditional flu season in 2020-2021, the number of influenza cases in that timeframe was historically low. Experts attributed this to social distancing and mask mandates.
In spite of this and the fact that many countries are still grappling with the far-reaching effects of the COVID-19 pandemic, a new health crisis is gaining steam: one where people test positive and get sick simultaneously with the flu virus and SARS-CoV-2.
How serious could this simultaneous infection with two life-threatening viruses get?
Symptoms To Expect
The flu and COVID-19 are both caused by respiratory viruses. Symptoms for both illnesses are similar and might include fever, headache, coughing, a runny nose, and a sore throat.
The loss of smell and taste are unique symptoms of positive COVID-19 cases.
Furthermore, COVID-19 can cause an infection in the lower part of the respiratory tract spreading to the lungs and potentially causing pneumonia. This disease manifestation is not common with the flu.
At the beginning of the COVID-19 pandemic, many physicians and caregivers were in the dark when it came to information about COVID-19. Although we know much more about the virus now, scientists are not sure how the flu virus and the COVID-19 virus interact or the physical symptoms or complications a dual-infection represents. This uncertainty makes the idea of a “twindemic” harrowing as we begin to see a surge in simultaneous infections.
A Case for Vaccines
The flu vaccine has been around for years now. Each year, a new flu vaccine is designed to combat the strain of the virus that is most likely to be dominant that year. Recent studies show that the flu vaccine can reduce the risk of illness by 40%-60%, depending on individual comorbidities.
Although there has been controversy surrounding breakthrough infections that happen even after a person is vaccinated against COVID-19, there is evidence that shows that vaccinated individuals are less likely to become severely sick, hospitalized or need mechanical ventilation, should they become infected.
Additionally, with both illnesses, disease severity generally increases with age and pre-existing health conditions.
Regardless of these factors, however, there is ample evidence to support the fact that getting vaccinated against both illnesses can reduce the chances that a person gets flu and COVID-19 at the same time.
How Can We Control The “twindemic”?
In a study published in the International Journal of Environmental Science and Public Health, researchers showed that the sustained spread of SARS-CoV-2 is directly linked with human behavior.
Thus, while social distancing and masking rules may be relaxed, it is important for individuals to gauge where implementing both of these strategies may be warranted. Handwashing—with soap and water or a hand sanitizer—will continue to be a powerful resource in keeping both viruses at bay.
As mentioned above, vaccinations can reduce disease spread and severity as well. To minimize one’s chances of contracting the flu or COVID-19, they should adhere to the CDC guidelines regarding when to receive the vaccines or boosters.
We need more research to understand the molecular consequences of interactions between SARS-CoV-2 and the flu virus, and multiplex testing is an invaluable resource. Multiplex testing interrogates the same sample for multiple pathogens helping physicians diagnose patients faster so a treatment regimen can be implemented quicker.
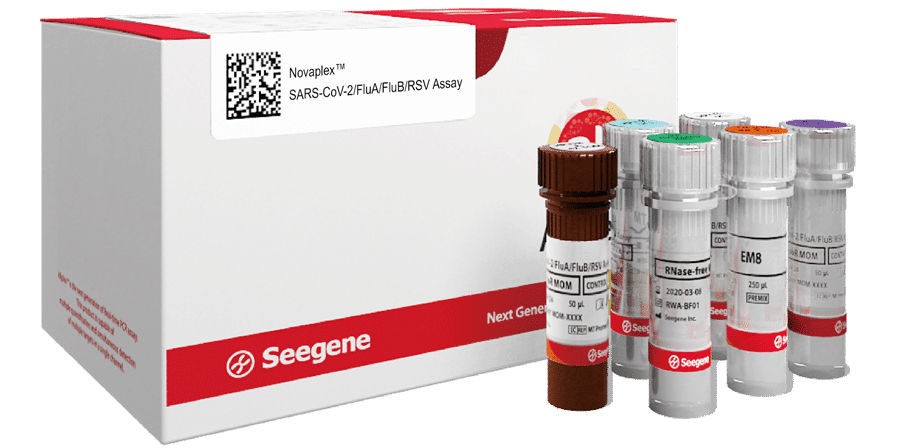
Seegene’s Novaplex™ SARS-CoV-2/Flu A/Flu B/RSV Assay is an essential tool in these research efforts. This assay is currently for Research Use Only (RUO) in the US, and not for use in diagnostic procedures. This multiplex, one-tube PCR test for SARS-CoV-2, Influenza A & B, and RSV is a simple way to confirm the presence of the virus, thus distinguishing it from illnesses with similar symptoms.
Other Blog Posts
Take a look at our other blog posts here: Seegene Technologies Blog Posts
